A Guide to the Remote ICU Model
In recent years, physician shortages have forced hospitals to get creative about patient care. One way in which they are doing this is by implementing ICU solutions such as a remote ICU model. This model has gained popularity particularly since the pandemic, when in-person care became dangerous for both patients and physicians. But, what exactly is the remote ICU model and how does it relieve staffing shortages? This guide has those answers.
Defining the Remote ICU Model
At its most basic, the remote ICU model uses off-site physicians and clinicians to collaborate with in-person ICU staff to consult on patient care and make patient care decisions. A remote ICU is not meant to replace in-person staff, which are needed for bedside care. Instead, it is designed to supplement in-person staff to give them additional resources to ensure their patients receive the best possible care.
The important element of a remote ICU, which is sometimes called a tele-ICU, is that the centralized off-site center that staffs the remote physicians and clinicians can be located anywhere so that even the most rural hospital can access the expertise of these professionals. Health information is securely exchanged electronically to the off-site staff to ensure all physicians and clinicians are on the same page regarding every patient in the care of the ICU.
How the Remote ICU Model Works
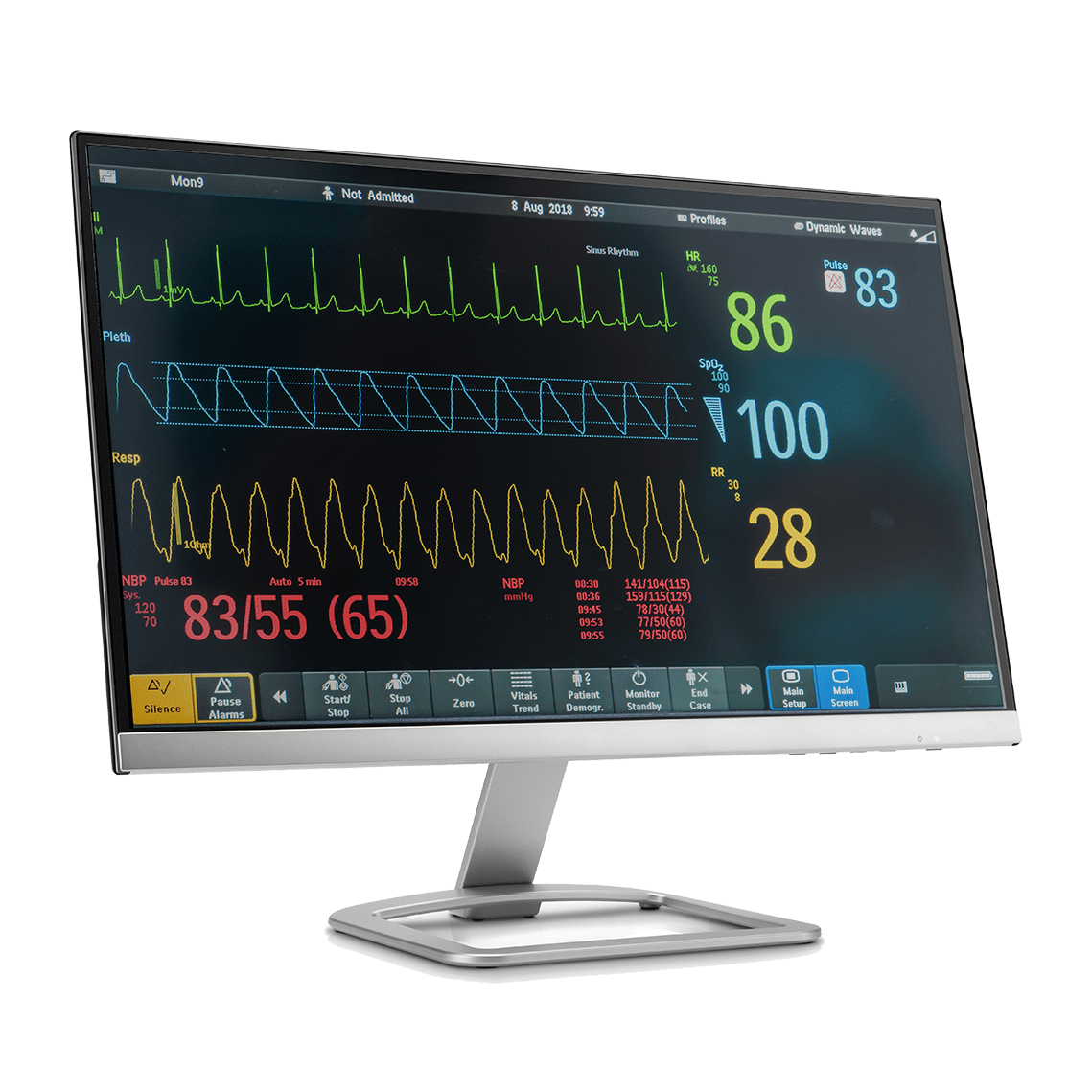
Technology makes the remote ICU model possible because the physicians and clinicians located in the off-site ICU can access live health information for each patient on monitors in the center. They are able to monitor patients’ vitals just as if they were next to them in the physical room to ensure they receive the proper medical treatment and interventions for their condition. If they detect an anomaly, they can alert the in-person staff to take action.
Audio-visual equipment and teleconferencing technology are also critical components of a remote ICU. Off-site physicians and clinicians are able to consult face-to-face with in-person staff to determine a course of treatment for a patient. They can also speak directly with patients and their families to explain their condition and treatment plan or get their consent for a specific procedure. Essentially, the physicians and clinicians in a centralized ICU can perform anything an in-person staff member can perform except the physical administration of treatment.
Benefits of the Remote ICU Model
Along with solving staffing shortages in ICUs and hospitals, a remote ICU has several additional benefits. The most important benefit of this model is that it improves patient outcomes. This is because someone is able to monitor all patients at all times. In-person staff can only do so much and unfortunately, things sometimes fall through the cracks. A tele-ICU closes those cracks and ensures all patients get the timely medical care they need, when they need it.
Additionally, a remote ICU ultimately costs less money for both the hospital and the patients. The hospital pays less for full-time ICU physicians and clinicians and spends less money on ICU services because patients don’t stay as long in a remote ICU as they have traditionally stayed in a regular ICU. This improvement in length of stay also lowers the patients’ bills as well.
Conclusion
Remote ICUs aren’t everywhere yet, but they soon will be more prevalent in hospitals everywhere as management begins to understand the multiple advantages they offer.